If you live in England, are under 25 and are sexually active, it's recommended that you get tested for chlamydia every year or when you change sexual partner.
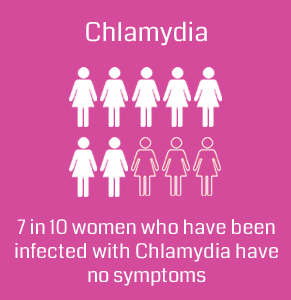
In 2013, more than 200,000 people tested positive for chlamydia in England. Almost 7 in every 10 people diagnosed with the condition were under 25 years old.
How do you get chlamydia?
Chlamydia is a bacterial infection. The bacteria are usually spread through sex or contact with infected genital fluids (semen or vaginal fluid).
You can get chlamydia through:
- unprotected vaginal, anal or oral sex
- sharing sex toys that aren't washed or covered with a new condom each time they're used
- your genitals coming into contact with your partner's genitals – this means you can get chlamydia from someone even if there is no penetration, orgasm or ejaculation
- infected semen or vaginal fluid getting into your eye
Chlamydia can't be passed on through casual contact, such as kissing and hugging, or from sharing baths, towels, swimming pools, toilet seats or cutlery.
Getting tested for chlamydia
Testing for chlamydia is done with a urine test or a swab test. You don't always need a physical examination by a nurse or doctor.
Anyone can get a free and confidential chlamydia test at a sexual health clinic, a genitourinary medicine (GUM) clinic or a GP surgery.
People under 25 years old can also get tested by the National Chlamydia Screening Programme (NCSP). This is often in places such as pharmacies, contraception clinics or colleges. If you live in England, you're under 25 and you're sexually active, you should get tested for chlamydia every year or when you change sexual partner, as you're more likely to catch it.
You can also buy chlamydia testing kits to do at home, such as Fujibio Chlamydia Test Kit. Unlike other home test kit available in the market today, it is clinically tested 99.9% accurate.
The one step Chlamydia test is a rapid qualitative immunoassay based on the immunochromatographic principle. (In the assay procedure, a clinical specimen is obtained and place into an extraction tube containing extraction solution. A. after two minutes. Extraction Solution B is added to the tube. 3 drops (approximately 150 ul) of extracted samples is added to the sample well).
The membrane is pre-coated with anti-genus specific lipopolysaccharide (LPS) monoclonal antibody on the test band (T) region and goat anti-mouse antibody on the control band (C) region. During testing, the sample is allowed to react with the colloidal gold particles which have been coated with monoclonal anti-chlamydia antibody, and then migrates laterally across the membrane by capillary action .
If the sample contains Chlamydia antigen , a colored band with a specific anti-body chlamydia antibody-mydia colloidal gold particle complex will form on the membrane in the test band (T) region. If Chlamydia antigen is not present, a pink line will only form on control band (C) region. To serve as a procedural control, a colored band at the control band (C) region will always appear regardless of the presence of Chlamydia antigen.
SPECIMEN COLLECTION AND HANDLING
The quality of specimen obtained is of extreme importance. Detection of Chlamydia requires a vigorous and through collection technique which provides cellular material rather than just body fluids.
For Female endocervical specimens:
The quality of specimen obtained is of extreme importance. Detection of Chlamydia requires a vigorous and through collection technique which provides cellular material rather than just body fluids.
For Female endocervical specimens:
- Before specimen collection, use a swab or cotton ball
to remove excess mucus from the endocervical area and discard.
- Use the swab provided with the kit or any shafted swabs
with rayon of Dacron tips. The swab should be interested into the
endocervical canal past the squamocolumnar junction, until most of the tip
is no longer visible. This will permit acquisition of columnar or cuboidal
epithelial cells which are the main reservoir of Chlamydia organism.
Firmly rotate the swab for 15-20 second and withdraw without contamination
of exocervical or vaginal cells.
- Alternative endocervical specimens can be collected
with a cytology brush (Not provided. Caution: do not use cytology brushes
with pregnant patients). Insert the cytology brush into the endocervical
canal past the squamocolumnar junction. Leave in place two to three
seconds. Rotate the cytology brush two full turns , and then withdraw the
brush without touching any vaginal surface.
- Place the swab in the extraction tube, if the test is
to be conducted immediately.
For Male Urethral Specimens:
- Use standard wire-shafted fiber-tripped swabs(not
provided) for urethral specimen collection.
- Instruct the patient not to urinate at least one hour
prior to specimen collection.
- Insert the swab into the urethra about 2-4cm, rotate
for 3-5 seconds and withdraw it.
- Place the swab to the extraction tube , if the test is
to be conducted immediately.
- Do not place the swab in any transport device
containing medium since transport medium inferences with the assay.
- If immediate testing is not possible, the patient
sample should be placed in a dry transport tube for storage or transport.
The swabs maybe stored for 4 hours at room temperature (10-30) or 24 hours
at refrigerated (4-8). Do not freeze. All specimens should be allowed to
reach a room temperature of 10-30 before testing.
TEST PROCEDURE
- Review ‘specimen collection’ instructions. Do not open
pouches until ready to perform the assay. Test reagents and specimen
should be brought to room temperature before testing.
- To avoid cross contamination, do not allow the tip of
the reagent bottle to come in contact with sample swabs of extraction
tubes.
A. Specimens and control extraction:
A1. Preperation of
endocervical or urethral swab specimens;
- Place a new extraction tube in the designated area of
the workstation. Add 6 drops of extraction solution A to extraction tube.
- Immerse the patient’s swab into the extraction tube,
and extracts 2 minutes at room temperature. During extraction, use a
circular motion to roll the swab against the side of the extraction tube
so that the liquid is expressed from the swab and reabsorbed.
- At the end of the extraction time, add 6 drops of
solution B. squeeze the swab firmly against the tube to expel as much
liquid as possible from the swab. Discard the following guidelines for
handling infectious agents.
- The extracted specimen can remain at room temperature
for 60 minutes without affecting the result of the Chlamydia test.
A2. Preparation of
positive and negative controls:
- Place a new extraction tube in the designated area of
the workstation. Add 6 drops of extraction solution A to extraction tube.
- Add two drops of the positive or negative control
solution to a sterile Dacron swab. Allow the swab to be absorbed into the
swab.
- Immerse the swab into the extraction tube, and extract
2 minutes at room temperature. During extraction, use a circular motion to
roll the swab against the side of the extraction tube so that the liquid
is expelled from the swab and reabsorbed.
- At the end of the extraction time, add 6 drops of
extraction Solution B. squeeze the swab firmly against the tube to expel
as much liquid as possible from the swab. Discard the swab following
guidelines for handling infectious agents.
B. Test Procedure:
- Follow instructions for specimen collections and
extraction.
- Remove the antigen test device from its protective
pouch and place it on a clean, dry, and level surface. Label the device
with patient or control identification.
- Place the cap of the extraction tube. Add 3 drops (approximately
150 ul) of extracted sample from extraction tube to the sample well.
- Wait for test band (S) to appear.the test results
should be read in 10 minutes after adding the extracted specimen to the
sample well. Depending on the amount of Chlamydia antigen organisms on the
swab, positive result maybe visible as soon as 1 minute, however to
confirm a negative result the complete reaction time of 15 minutes if
required. Do not interpret result after 15 minutes.
Invalid:
- No line appears in the control region. Under no circumstances should a positive sample be identified until the control line (C) forms in the viewing area. If the control line does not form, the test result is inconclusive and the assay should be repeated.
How chlamydia is treated
Chlamydia can usually be treated easily with antibiotics. You may be given some tablets to take all on one day, or a longer course of capsules to take for a week.
You shouldn't have sex until you and your current sexual partner have finished your treatment. If you had the one-day course of treatment, you should avoid having sex for a week afterwards.
It's important that your current sexual partner and any other sexual partners you've had during the last six months are also tested and treated to help stop the spread of the infection.
The NCSP recommends that under 25s who have chlamydia should be offered another test around three months after being treated. This is because young adults who test positive for chlamydia are at increased risk of catching it again.
Sexual health or GUM clinics can help you contact your sexual partners. Either you or the clinic can speak to them, or they can be sent a note advising them to get tested. The note won't have your name on it, so your confidentiality will be protected.

Hello everyone, I want to say a special thanks to Dr OGU. for helping me get cured from herpes virus 2019 , I contacted him base on the testimonies I saw about him on the internet I was diagnosed of HERPES Virus i have tried all I can to get cured but all to know avail, until i saw a post in a health forum about a herbal man who prepare herbal medication to cure all kind of diseases including HERPES virus, at first i doubted if it was real but decided to give it a try I was cured by his herbal medicine and natural herbs, kindly contact him today through his email: drogugusolutionhome@gmail.com or text/call: +1 (719) 629 0982
TumugonBurahinHe’s waiting to help you.
HE ALSO SPECIALIZE IN THE FOLLOWING Illness;
If you have any sickness like : H I V/AIDS , CANCER , HERPES 1 or 2 , GENITAL WARTS (HPV), Chlamydia, Hepatitis B. Trichomoniasis Gonorrhea, Epilepsy, and Syphilis.
Naalis ng may-ari ang komentong ito.
TumugonBurahin